What is Fibromyalgia

|
Buddha |
Are you suffering from chronic, widespread body discomfort and fatigue? After waking up do you still feel tired and groggy? Do you often find it difficult to focus and concentrate? You're not alone. Everyday millions of Americans suffer these symptoms commonly associated with Fibromyalgia. Chronic, widespread body discomfort robs you of the lifestyle you deserve. It takes a toll on your family, friends, and career, leaving you feeling helpless and frustrated.
Fibromyalgia is not a new condition. It's been around for centuries with people reporting conditions with similar symptoms through the ages. But Fibromyalgia wasn't officially given its current name until 1976. Doctors have officially been studying the condition since the 1800s and in 1816 University of Edinburgh surgeon, Dr. William Balfour, gave the first medical description of fibromyalgia. In 1824 he identified the described tender points and what they are. Symptoms of fibromyalgia were called muscular rheumatism in the 1600s. In 1904 the name to describe the symptoms was changed to fibrositis by Sir William Gowers to recognize the tender points that patients with muscular rheumatism experienced.
The foundation for the name fibromyalgia was laid in 1972 when Dr. Hugh Smythe began describing the widespread pain associated with the tender points. The sleep disturbances associated with fibromyalgia was discovered in 1975. Further studies by medical researchers discovered that inflammation didn't occur around the tender points and the name of the condition was changed from fibrositis to fibromyalgia, which means pain in muscles and tissues. In 1987 fibromyalgia was considered a real physical condition by the American Medical Association. Three years later in 1990 the American College of Rheumatology developed diagnostic criteria for the condition to help doctors diagnose patients with fibromyalgia.
Studies in the 20th century began when the condition was considered a real illness. Tests were done on the muscles and tissues of patients to see if there was any damage to them. No damage was discovered leading researchers to theorize FM was an autoimmune disorder. Studies showed that FM does not disturb the immune system.
Even though fibromyalgia is frequently referred to as an arthritis-related condition, it does not cause joint damage or inflammation, as arthritis does. Neither does fibromyalgia cause damage to muscle and other tissues. However, it is similar to arthritis because it causes severe pain and tiredness, and can undermine the patient's ability to go about his daily activities.
The term "fibromyalgia" derives from new Latin, fibro-, meaning "fibrous tissues", Greek myo, "muscle", and Greek algos, "pain"; thus the term literally means "muscle and connective tissue pain".
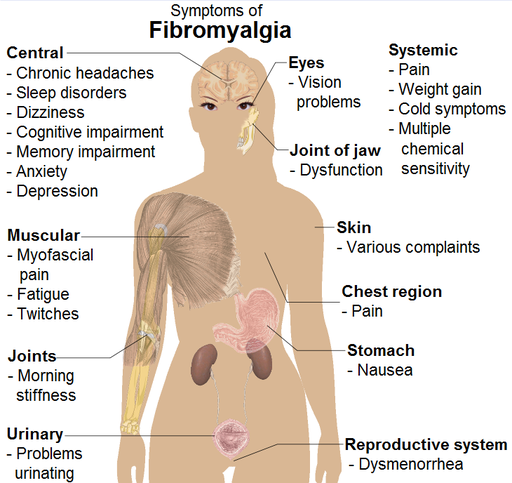
Fibromyalgia is a chronic disorder characterized by widespread pain and morning stiffness in your muscles, ligaments and tendons as well as sleep difficulties, depression, anxiety, memory lapses and difficulty concentrating. Researchers believe fibromyalgia affects your brain and amplifies pain sensations.
Some patients may also report difficulty with swallowing, IBS (irritable bowel syndrome), headaches, painful menstrual periods, bladder abnormalities, restless leg syndrome, vision, skin problems, weight gain, chest pain, numbness and tingling, sensitivity to cold or heat, cognitive dysfunction and others. Not all people with fibromyalgia experience all associated symptoms.
 |
Fibromyalgia is estimated to affect 2–4% of the population, with a female to male incidence ratio of approximately 9:1. Fibromyalgia occurs along with other rheumatic diseases such as Lupus and Rheumatoid Arthritis 25-65 percent of the time. |
Diagnosis can take on average five years with 60 percent of fibromyalgia patients diagnosed in their 30s and 40s, another 35 percent diagnosed in their 20s or between the ages of 50-65.
The majority of people diagnosed with FMS really have chronic fatigue syndrome, except they experience more intense muscle pain along with fatigue. Chronic Fatigue Syndrome (CFS) is the disease with persistent fatigue lasting for six months or more. People with CFS have exhaustion so severe and persistent that normal activity is impossible. The pain of fibromyalgia is often so severe; it brings people into depression and sometimes even suicide.
Most people with fibromyalgia complain of pain over many areas of their body, with an average of six to nine locations. Although the pain is frequently described as being "all over," it is most prominent in the neck, shoulders, elbows, hips, knees, and back. Tender points are generally symmetrical and on both sides of the body. The areas of tenderness are usually small (less than an inch in diameter) and deep within the muscle. They are often located in sites that are slightly tender in normal people.
Patients with fibromyalgia have pain in at least 11 of the following 18 tender point sites
(one on each side of the body):
- Base of the skull where the suboccipital muscle inserts
- Back of the low neck (anterior intertransverse spaces of C5-C7)
- Midpoint of the upper shoulders (trapezius)
- On the back in the middle of the scapula
- On the chest where the second rib attaches to the breastbone (sternum)
- One inch below the outside of each elbow (lateral epicondyle)
- Upper outer quadrant of buttocks
- Just behind the swelling on the upper leg bone below the hip (trochanteric prominence)
- The inside of both knees (medial fat pads proximal to the joint line)
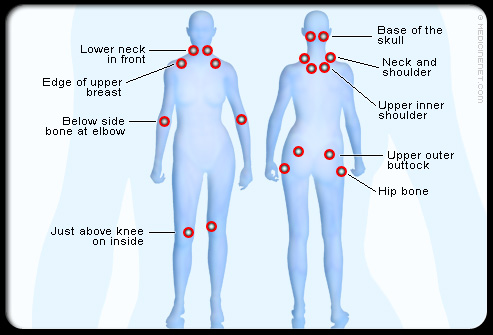 |
People with fibromyalgia, however, differ in having increased tenderness at these sites from the average person. |
Firm palpation with the thumb (just past the point where the nail turns white) over the outside elbow will typically cause a vague sensation of discomfort.
Patients with fibromyalgia will experience much more pain and will often withdraw the arm involuntarily.
More than 70 percent of patients describe their pain as profound aching and stiffness of muscles. Often it is relatively constant from moment to moment, but certain positions or movements may momentarily worsen the pain. Other terms used to describe the pain are "dull" and "numb."
Sharp or intermittent pain is relatively uncommon.
Patients with fibromyalgia also often complain that sudden loud noises worsen their pain.
The generalized stiffness of fibromyalgia does not diminish with activity, unlike the stiffness of rheumatoid arthritis, which lessens as the day progresses. Despite the lack of abnormal lab tests, patients can suffer considerable discomfort.
The fatigue is often severe enough to impair activities of work and recreation. Patients commonly experience fatigue on arising and complain of being more fatigued when they wake up than when they went to bed.
Over 90 percent of patients believe the pain, stiffness, and fatigue are made worse by cold, damp weather. Overexertion, anxiety, and stress are also factors. Many find that localized heat, such as hot baths, showers, or heating pads, give them some relief. There is also a tendency for pain to improve in the summer with mild activity, or with rest.
Some patients will date the onset of their symptoms to some initiating event. This is often an injury, such as a fall, a motor vehicle accident, or a vocational or sports injury. Others find that their symptoms began with a stressful or emotional event, such as a death in the family, a divorce, a job loss, or similar occurrence.
Fibromyalgia patients seem to feel more intense pain, and though it’s not understood why. There is some research that helps explain why. Scientists think that it begins in the deep tissues of the muscles and joints with a tightening of muscles.
Muscles hypertension leads to changes in signal of central nervous system and changes in neurotransmitter activities. The level of substance P (a neurotransmitter responsible for the chronic pain conduction through the spinal cord) increases and the level of serotonin decreases. Serotonin is a very important neurotransmitter, mediating basic bodily functions such as smooth muscle contraction (especially digestive system musculature) and blood coagulation. Additionally, serotonin acts as a neurotransmitter in the brain. It is responsible for our wakeful state and excitement. Patients with clinical depression, which frequently accompanies FM, show a significant decrease in the concentration of serotonin in the brain. All examined FM patients exhibit an increase in the concentration of substance P in the spinal cord, which in most cases is the result of a decreased pH level in muscles.
Important findings supporting this theory are pathological changes found in the muscle cell mitochondria, as well as a decrease in magnesium concentration. Mitochondria are the power plants of the cell, synthesizing ATP (magnesium is a mediator in ATP synthesis). Numerous mitochondria are found within each cell. When ATP is depleted in the skeletal muscles of FM patients, an "energy crisis" is created, triggering the entire clinical picture.
Tightening of muscles leads to poor sleep. Without proper rest, the muscles can’t recover, and this can lead to continuous signals between your muscles and your central nervous system. Then this alters the way that your central nervous system processes outside conditions. You will feel more pain and be more sensitive. This is known as central sensitization.
An interesting thing about central sensitization is that the causes and effects of fibromyalgia are thought to be bidirectional. This means that structural imbalances can cause your muscles to tighten, while tight muscles can lead to structural imbalances. In addition, poor sleep can lead to your muscles tightening, and tight muscles can lead to poor sleep. You get the idea and can see the vicious cycle, right? How can you stop this cycle?