Interstitial Cystitis

|
Voltaire |
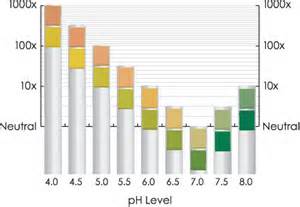
Interstitial cystitis affects more than 1.2 million people in the United States, 90% of whom are women. Interstitial cystitis can affect women at all stages of life, from puberty to menopause, all of which have unique challenges with this condition. It is important to understand that our hormones, particularly estrogen, play a large role in managing (or even preventing) the inflammation that relates to IC. Even though the symptoms can feel similar to a urinary tract infection (UTI), but this condition won’t show up on regular urine cultures for bacteria and other pathogens. Unfortunately, taking antibiotics won’t help either. Nor will drinking more cranberry juice — natural UTI treatments can in fact make IC symptoms worse.
Interstitial cystitis can be downright unbearable for some women, preventing them from going to school, work, or participating in any of their normal day-to-day activities, not to mention making their sex lives very painful. Too often women just “live with it” for years before looking for help. Or a woman could see up to five different practitioners over the course of many years before being accurately diagnosed with interstitial cystitis!
The symptoms of IC are easily confused with a wide range of other problems, from bladder infections (UTI’s) and urge incontinence to bladder cancer, endometriosis, STD’s, and kidney stones. These disorders have different root causes and need different types of treatments. A lot of women with IC see their healthcare practitioners thinking they have a UTI and are told their urine is “clean” — that means on culture that no abnormalities were seen in the urine when it was evaluated in the lab.
you we’ll learn about:
- What are symptoms and causes of interstitial cystitis
- What is the difference between UTI and IC
- What is the link between chronic interstitial cystitis and estrogen, and menopause